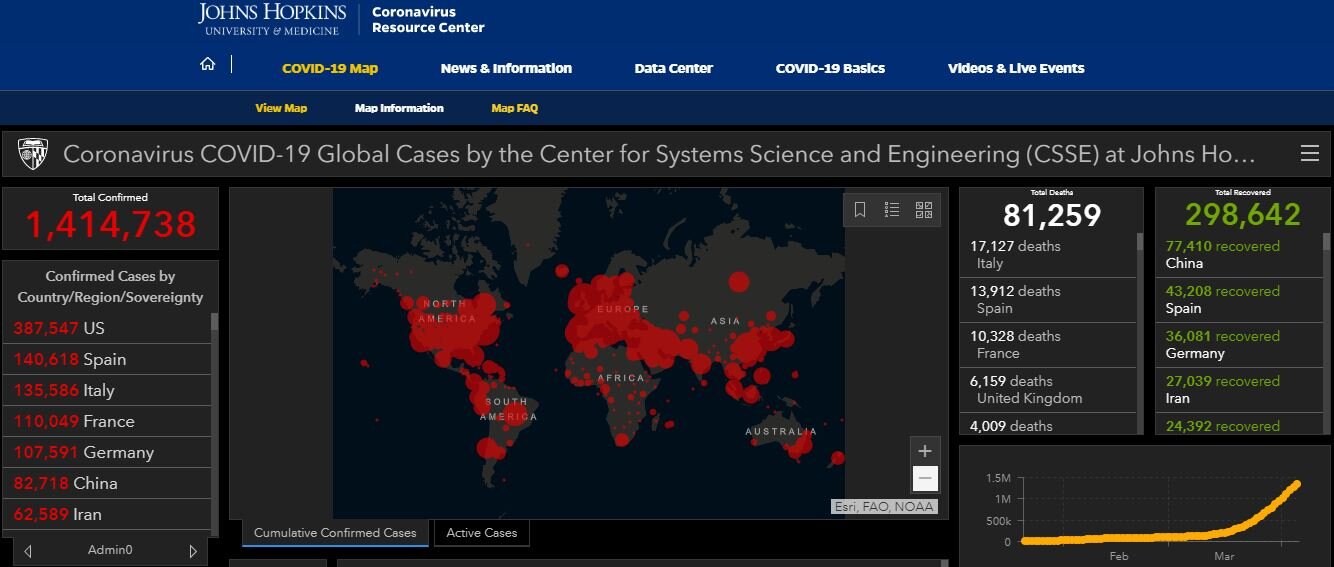
There were 6000 cases in the world, 200 deaths and 5 cases in the US. Today the story is very different. Here are today’s data (likely a large underestimate):
CO has reported 5,172 total cases, 150 deaths, 39 confirmed cases in Pitkin County.
FLATTENING THE CURVE:
Most governments have ordered strict restrictive policies, shutting down all non-essential business, forbidding travel between and within countries, and issuing shelter at home orders. China has seemed to contain and stop viral spread using these methods, South Korea has done the same using a containment strategy of intensive testing then tracking contacts and isolating them. Spain and Italy may finally be bending the curve after much devastation. Germany has also rolled out much testing and containment of cases, so their cases and deaths have not been as severe as other European countries. Finally, the US may be in the very early stages of bending the curve.
How well is the US flattening the curve?
Deaths could peak in mid April
TESTING (The hottest topic in COVID-19 today) WILL HELP BEND THE CURVE MUCH FASTER:
There are two types of tests-
1. Testing for the acute presence of SARs-CoV-2. Making and distributing an adequate number of these tests with quick turnaround time has pretty much been a disaster in the US due to regulatory issues, lack of supply chain for reagents, the CDC test being faulty for too long, and lack of manpower to perform specimen collection as well as logistical bottlenecks in performing the tests in labs. However, now dozens of these types of tests have very recently received emergency use approval by the FDA.
Current testing is generally sent to a central lab for processing with a turnaround time of days, a few newer ones enable Point of Care (POC) testing which can give either a positive or negative result in as little as under an hour. However, the sensitivity of many of these tests is only 65-70%, meaning lots of false negatives. Variables such as the method of collection, timing of the appearance and clearance of the virus in the human respiratory tract, and the performance characteristics of the tests themselves are responsible for the low sensitivity. Therefore, we cannot be over reliant on these tests to confirm COVID-19 or not.
2. The second type of testing getting much press lately are the antibody tests (serologic). Animals make immune responses to pathogens such as viruses and these responses are generally measured by looking at levels of antibodies (Immunoglobulins-Ig) in the blood. IgM is generally indicative of a rapid or acute response, usually seen within 2-6 weeks after an infection, they diminish; IgG levels rise later and can stay high for some time, even a lifetime.
These tests are going to be crucial to determine who in a population has been exposed, infected, and is (hopefully) immune. But we don’t quite know yet which antibodies, if any, will indicate short- or long-term immunity. There is a huge worldwide race on to figure this out and validate findings. Based upon SARS1 and MERS antibody data immunity to COVID-19 is expected to last 2-3 years.
TESTING IN THE ROARING FORK VALLEY: AVH has adopted a policy of testing only very severely ill people that need hospital admission with the acute test. To fill the gap, several providers in the Roaring Fork Valley are offering these tests. I offer testing through LabCorp. Another provider can do large numbers of tests though tests are being reserved for patients with symptoms or health care providers. So please, give me a call if you are sick and interested in this. I will also shortly have the antibody testing available through LabCorp.
TAKE HOME MESSAGES:
Symptoms are commonly fever, cough, shortness of breath but can be just minor cold-like, diarrhea, headache, and achiness, as well as loss of taste and smell.
Most cases are likely to be mild and self-limited (80%+); children especially tend to have milder illness.
At present the mortality from 2019-nCoV appears to be 1-2% in the US.
The median age of cases is 47-59 years; about 57% of infections are in men. The elderly and people with underlying health conditions are at highest risk for dying: 15% in those over 80; but this can be a very dangerous disease at ANY age. Many young healthcare workers and first responders without health issues have died from COVID-19.
We are still not sure why some people get sick and die and others seem so resistant, i.e., why is the death rate in Italy so high? It’s not just age. Scientists are researching possible
the “R0” or spread rate appears to be about 2.5; that is, without physical distancing, for each case an average of 2.5 additional people will get COVID-19.
Time from being exposed to getting signs are median of 5.1 days, can be 2-14 days. We now know people can be transmitting the virus while they are asymptomatic and in fact may be most contagious during that time!
Research shows that SARS2-CoVID2 viral RNA is detectable in the air for up to two hours and on some surfaces for up to three days after shedding occurs. The virus is shed in stool for a month or more. Whether any of this is live virus able to infect again is unknown at this point.
Handwashing continues to be a hallmark of reducing spread. The CDC now recommends use of masks by everyone all the time when in public.
Treatment is largely supportive but some old meds like HYDROXYCHLOROQUINE and Remdesivir appear promising. The WHO is launching a huge randomized trial (Solidarity) of the four most promising treatments. In the meantime, hospitals in the US are treating sick people with hydroxychloroquine and Remdesivir, among others, when available. Using serum from people who have recovered from COVID-19 anecdotally works.
The first US vaccine trial started several weeks ago in SEATTLE. Other trials have also recently started. Bill Gates announced that he will be setting up funding for 7 laboratories testing the 7 most promising vaccines, developing and testing in parallel. This is costing billions of dollars.
Because SARs-CoV-2 attaches to human respiratory cells through the ACE2 (angiotensin converting enzyme 2) receptor, there is speculation that use of ACE-inhibitors and ARBs (angiotensin receptor blockers), which can upregulate the ACE2 receptors, could be harmful—though there is no data on this yet. Other scientists feel those medications may be helpful. Stay on all your prescribed meds including ACE=inhibitors (i.e., lisinopril—the “prils”) and Angiotensin Receptor blockers (the ARBS—like losartan) until you check with your physician. There is no evidence that these should be stopped to prevent or treat COVID-19.
Ibuprofen has NOT been shown to be unsafe in COVID-19 per se, however, some people will have contraindications to using NSAIDs (i.e., kidney disease, clotting issues, liver problems) and some people prefer not to take the risk. That’s fine: use acetaminophen instead for fever and aches.
Call us if you develop signs of COVID-19 or
have questions about getting tested!